 accines against SARS-CoV-2 are starting to undergo clinical testing, and we all
hope they'll be safe and effective. But how is that done? And what are the risks?
accines against SARS-CoV-2 are starting to undergo clinical testing, and we all
hope they'll be safe and effective. But how is that done? And what are the risks?
Creating a vaccine is not simply a matter of whipping up a batch of viruses, injecting patients, and seeing if they work. The challenge is to create something that works harmoniously with our immune systems. But immune systems don't need vaccinations to go haywire. They can go haywire all by themselves, and this tells us a lot about the challenges virologists face.
A classic example is dengue hemorrhagic fever. Dengue fever is a mosquito-borne viral disease characterized by high fever, rash, headaches, and bone pain. The symptoms disappear after a week or so. But if the patient is exposed a second time, they can get a much more severe disease called dengue hemorrhagic fever, in which the capillaries are weakened and massive bleeding occurs, leading to shock. This can also occur with yellow fever, another mosquito-borne viral disease.
Although there is still some debate about the exact causes, many immunologists think dengue hemorrhagic fever happens because the body produces antibodies that bind to the virus but don't neutralize it. This can happen if the antigenic sites on the virus that produce the strongest antibody response happen to be sites that aren't important for the virus to function. Instead of tagging the virus for destruction, the antibody might actually help the virus enter the cell. This is called antibody-dependent enhancement or ADE.
ADE is a property that's shared by many enveloped viruses, including SARS coronavirus and SARS-CoV-2. To prevent this, vaccine manufacturers will have to focus exclusively on making antibodies against the receptor-binding domain of the SARS-CoV-2 spike protein.
Another challenge to overcome is that an antigen, whether on a virus protein or a badly designed vaccine, can sometimes produce an autoimmune response—which is very bad. The classic example of this is measles virus, in which a small minority of children who recover from measles get a brain infection called acute disseminated encephalomyelitis, which causes seizures, ataxia, hemiparesis, and a sudden decrease in verbal output or even mutism that begins a few weeks after an infection. Now that measles is rare thanks to the MMR vaccine, this disease is uncommon, but it can still happen after an upper respiratory infection.
NMDA receptor encephalitis
Another autoimmune disease is NMDA receptor encephalitis, where the patient produces antibodies against their own NMDA receptors. NMDA receptors are proteins in the brain that control neuronal signaling from glutamate, which is the predominant neurotransmitter in the brain. The patient gets a low-grade fever, headache, and flu-like symptoms, which progress to psychiatric symptoms such as agitation, bizarre behavior, delusions, and hallucinations—collectively called psychosis—and then to seizures and coma.
NMDA receptor encephalitis is classically caused by an autoimmune response to a cancerous tumor. But it can also be triggered by a virus. Although only discovered in 2007, it is one of the most common virally-caused neurological entities in pediatric patients.
Autoimmune reactions to COVID-19
So far, not much is known about autoimmunity after COVID-19. As I described here, influenza, SARS-CoV, and other viral respiratory diseases are well known to cause psychosis and neurological dysfunction that becomes manifest weeks or months after the patient recovers. Once again, an autoimmune response is suspected, but cytokine release syndrome and possibly vascular endothelial dysfunction in the blood capillaries may also play a role.
As many people know, COVID-19 causes many neurological problems including anosmia (loss of smell), confusion / delirium (65%), PTSD (32%), depressed mood (10%), and anxiety (12%). There have also been a few cases of acute mania[1]; 12% of patients get irritability, and about 0.7% of patients get steroid-induced mania and psychosis[2]. There are even a few reports of patients getting a type of paralysis called Guillain-Barré syndrome or another autoimmune reaction called immune thrombocytopenic purpura.
Kawasaki-like syndrome in children is not technically an autoimmune disorder but an overreaction of the innate immune system, which produces cytokines, although Kawasaki patients also have a deficiency of regulatory T (Treg) cells. This can happen in pediatric COVID-19 patients[3], which attacks Treg cells and resembles an immunodeficiency disease in some ways.
Vaccine Engineering
There are no effective vaccines for many diseases including HIV, malaria, and tuberculosis. Part of the reason is that vaccination induces the body to create antibodies (which are made by B cells), but it's comparatively ineffective in producing cell-mediated immunity, such as that mediated by CD8+ T cells. If the pathogen evades the antibody, possibly by getting inside the cells before the antibody can reach it, or (in the case of HIV) knocking out the T cells altogether, vaccination might not work. Another complication is that there are some viruses that antibodies are unable to neutralize, because there are too many different strains or clades, which means many different antibodies would be needed.
For years, most vaccines against viruses have been made by designing genetically attenuated pathogens. This is traditionally done by growing the virus in non-human cells, which weakens their ability to infect humans. Live viruses are necessary because killed viruses cannot infect cells and therefore don't efficiently generate cytotoxic CD8+ T cells. The CD8+ T cells depend on MHC class I presentation of degraded virus proteins to identify and kill cells that are infected—an amazingly clever way nature has devised for the T cell to see what's inside another cell—which antibodies can't do. For cellular immunity to happen, the part of the antigen (called an epitope) that's visible to the T cell has to match the part that's recognized by the B cell.
But giving a patient attenuated viruses can be risky. One risk is that the virus could mutate and become pathogenic again. Another is that if two different viruses mix within the same cell in a patient, they could (in principle) recombine, producing an altered virus with effects that are hard to predict. A new approach is to engineer the virus using recombinant DNA technology to make it virtually impossible for the virus to mutate. This could be used to create an efficient killed influenza vaccine—a desirable goal because influenza vaccines have had to rely on killed viruses, which are less efficient than attenuated ones.
Some vaccines against bacterial infections consist of purified bacterial proteins instead of whole organisms. These acellular vaccines often need an adjuvant to make the protein immunogenic enough. In the USA, only inorganic aluminum salts are approved as adjuvants. These salts are thought to stimulate the innate immune system, which permits lower doses of antigen to be used.
There are many scientific articles speculating on possible toxic effects of aluminum. Not all of them are reliable. For example, most Alzheimer researchers dismiss claims aluminum could cause Alzheimer's disease, because aluminum intoxication produces a different set of symptoms than Alzheimer's. There are many forms of aluminum ranging from harmless oxides to insoluble metals, some of which can cause toxic effects, so when reading the papers it is always necessary to ask what doses were given, what chemical form was used, how much was absorbed, and how reliable were the tests that were used. Aluminum is not a simple topic to study, and it has attracted a lot of poor quality science.
But what if we could use cellular engineering to provide the patient with ready-made B cells or dendritic cells that produce perfectly designed antibodies and perfect cytotoxic T lymphocytes that do exactly what we want?
Doing so would have some great advantages:
- It would build up immunity faster than a vaccination, because an optimal number of cells could be injected and the lymphocytes could be engineered to detect the antigen with high specificity.
- Unlike vaccination or natural immunity, which runs the risk of producing non- neutralizing antibodies, the injected T cells would be designed expressly to efficiently eliminate cells presenting the pathogen while being engineered not to produce an autoimmune response.
- Adjuvants could be greatly reduced or eliminated.
This approach is too expensive and labor-intensive at present, but as precision medicine advances it could someday be commonplace.
Immunotherapy
Immunotherapy, where we inject a pre-made synthetic or cloned antibody, is a different way of dealing with a virus. Immunotherapy can be a highly effective treatment for patients, but it cannot prevent infection. As with a vaccine, the antibody still has to be tested for safety to avoid triggering the recipient's own immune response. This has happened in the past with antibodies against respiratory syncytial virus and antibodies against beta-amyloid protein for Alzheimer's.
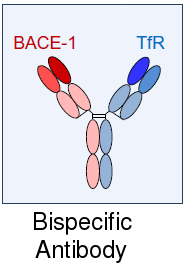
A bispecific antibody binds to two different proteins
Companies are also experimenting with bi-specific antibodies, which can bind to two different antigens and link them together. They're also experimenting with antibody fragments, which are cheaper to manufacture than conventional antibodies. These are things that never occur in nature, and the possibilities are enormous.
Of course, being corporations, they're mostly trying to do crazy things like using antibodies to get their most profitable drug across the blood-brain barrier to treat brain disorders like Parkinson's disease. But eventually they may start doing more imaginative things that could benefit patients.
In the future, it might even be possible to engineer non-living nanoparticles or living dendritic cells that could induce the immune system to make antibodies and T cells against specific antigens much more efficiently and with lower risk.
One of the biggest challenges is that some viruses, such as HSV-2, become latent, which means their DNA gets incorporated into the patient's DNA, making it inaccessible to the immune system. Perhaps someday we will know how to use gene therapy tools such as Crispr to clear these latent viruses.
None of these things would have been possible if not for the Human Genome Project. Those who say it was a waste of money need to look into what's happening more closely. It has become the basis for almost everything that is done in biology.
1. Mawhinney JA, Wilcock C, Haboubi H, Roshanzamir S (2020). Neurotropism of SARS-CoV-2: COVID-19 presenting with an acute manic episode. BMJ Case Rep. 2020 Jun 14;13(6). pii: e236123. doi: 10.1136/bcr-2020-236123.
2. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020 May 18. pii: S2215-0366(20)30203-0. doi: 10.1016/S2215-0366(20)30203-0.
3. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, Xie C, Ma K, Shang K, Wang W, Tian DS. (2020). Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. Mar 12. pii: ciaa248. doi: 10.1093/cid/ciaa248. PMID: 32161940 PMCID: PMC7108125
jun 19 2020, 8:33 am
