 t may surprise you to learn that DNA therapy has been in use since the 1990s.
It's not just genetically engineered CAR-T cells and cloned antibodies. Now
scientists have invented a new way to make vaccines using DNA that promises
to be faster, cheaper, and safer.
t may surprise you to learn that DNA therapy has been in use since the 1990s.
It's not just genetically engineered CAR-T cells and cloned antibodies. Now
scientists have invented a new way to make vaccines using DNA that promises
to be faster, cheaper, and safer.
These are called DNA vaccines. As often happens, when people hear the term DNA, they imagine movies like Hanna, where Saoirse Ronan ran around trying to escape from rogue CIA agents who deleted her FOXP2 gene to give her super-frizzy hair.
But unlike that elusive hair-frizziness gene, it turns out that DNA vaccines are exactly what anti-vaxxers have always wanted. They eliminate the need for thiomersal and reduce the need for adjuvants. They eliminate the need to use weakened pathogens and serum. And they allow doctors to make vaccines safer, more specific, and faster than ever.
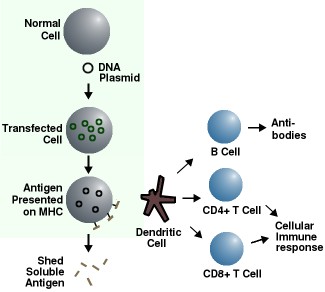
DNA Vaccine. DNA plasmids are inserted into the cytoplasm of cells near the injection site. The cells then use the DNA to express the antigen. The antigen can either be shed as a soluble protein, as would happen with a normal vaccination, or it can be presented on the MHC (major histocompatibility complex), which stimulates the immune response. The green part is unique to DNA vaccines.
Once the protein is degraded and expressed on antigen-presenting cells (APCs) such as dendritic cells, the cells travel to the lymph node and initiate a potent immune response. Expressed antigen can also be shed extracellularly and picked up by other APCs. Extracellular antigen can also induce a B-cell response, producing antibodies in much the same way as an ordinary vaccine.
In an ordinary, everyday vaccine, the antigen—typically a protein or inactivated virus—is injected into your muscle. This causes your immune system to identify it as a foreign molecule, and your B cells make antibodies against it. Conventional vaccines rely mainly on the B cell response, while barely engaging the cell-mediated immune response, which also involves T cells and cytokines as a real infection would.
But because antigens are proteins, they get chewed up by proteases in our bloodstream and elsewhere. They take time to manufacture and they have to be kept cold to avoid losing their effectiveness. And they require an adjuvant to encourage the immune system to respond.
In a DNA vaccine, a piece of DNA from, say, a virus surface protein is put into a plasmid, which is a circular piece of double-stranded DNA. Because the plasmid does not contain integrase or recombinases like Cre (as in Cre-Lox), it cannot integrate itself into your cells' genome. In fact, the plasmid is designed not to replicate at all. Instead, it's translated into RNA in the nucleus and then expressed as protein. Once your cells at the injection site take up the plasmid, they will use it as a template to manufacture proteins or peptides on their own, just as if your body had caught the disease. Your cells then degrade the protein, making peptides, and present them on the cell surface via the major histocompatibility complex-I or II (MHC-I or II) as usual.
This is called antigen presentation. When antigen is presented by MHC class II proteins, which are found on dendritic cells, B cells, and mononuclear phagocytes, it activates CD4+ helper T cells. These cells are called professional antigen-presenting cells. When antigens are presented by MHC class I proteins, which are on the surface of most other nucleated cells, they activate cytotoxic CD8+ T cells, which are important for viral clearance. (Mnemonic: 1×8 = 2×4)
As shown in the figure, once your immune cells come along and bind to the MHC protein, they initiate an immune response in the lymph nodes against the peptide the MHC protein is carrying.
An early whole-body electroporation experiment
Note that the plasmids don't code for antibodies. They're only an efficient way of giving an antigen. When recombinant plasmids were first invented, scientists had to take elaborate precautions with them, because it was feared that they'd get out of control. But it was soon realized that bacteria don't like plasmids and automatically throw them out because they use the bacteria's resources without providing any survival advantage.
For bacteria, plasmids are like sex: conjugation is how they exchange genetic material with each other, so they take up plasmids spontaneously. Eukaryotic organisms have discovered better ways of exchanging DNA, which we learn about in grade school when they teach us how to put condoms on aubergines. So mammalian cells don't take any old DNA that they find lying around and stuff it into their genome. If they did, gene therapy would be easy. To get it into the cells, your doctor might use a technique called adaptive electroporation, which involves creating a local electric field around the cells that makes temporary holes in the cell membrane that allow the DNA to enter. Electroporation is said to improve uptake by 500×.[1] Once a plasmid gets into the cell, it then has to get into the nucleus, which is almost as hard to do.
It's thought that the best vaccination route is intradermal, because the epidermis has many professional cells called dermal dendritic cells, dermal macrophages, and especially Langerhans cells, which routinely travel to the lymph node and present antigen.[3] New intradermal injection methods using micro-needle arrays are less painful than previous methods, and intradermal injection uses lower injection volumes than other sites.
To anti-vaxxers, all this probably sounds like they'll be strapped to a table and raised to the roof during a thunderstorm so alien DNA can be zapped into their brain. Or maybe they'll have to be gagged and strapped down to prevent them from biting their tongue as mutant DNA is forced into their cells. But the alternative is a gene cannon—or worse, a gene suppository[4]—so they better not complain.
Of course, it will be nothing like that unfortunate Frankenstein experiment. It'll be more like a tiny electric current like you'd get from walking across a carpet.
DNA vaccines are being created for Venezuelan equine encephalitis virus, for which there are no approved vaccines or therapeutics. DNA vaccines for influenza, HIV, Zika virus, HPV, and MERS-CoV also nearing clinical trials. Influenza is probably the most important one: current vaccines are inefficient and hard to produce, and influenza causes 290,000–650,000 deaths annually.[2]
Because they're disease specific, DNA vaccines won't replace small molecules like antivirals, and there are still technical challenges to overcome before they can replace ordinary vaccines. And we can probably never stop conspiracy theorists from making up scary stories. Their stories might be more interesting, but DNA vaccines are about as boring and as un-scary as you can get.
1. Gary EN, Weiner DB (2020). DNA vaccines: prime time is now. Current Opinion in Immunology 65, 21–27. https://doi.org/10.1016/j.coi.2020.01.006
2. Lee LYY, Izzard L, Hurt AC (2018). A Review of DNA Vaccines Against Influenza. Front Immunol. 9, 1568. doi: 10.3389/fimmu.2018.01568.
3. Combadiere B, Liard C (2011). Transcutaneous and intradermal vaccination. Human Vaccines, 7:8, 811–827, doi: 10.4161/hv.7.8.16274
4. Babiuk LA, Pontarollo R, Babiuk S, Loehr B, van Drunen Littel-van den Hurk S (2003). Induction of immune responses by DNA vaccines in large animals. Vaccine 21(7–8), 649–658.
apr 16 2020, 10:04 am
