t is hard to overstate the significance of the new results on Alzheimer's disease
that have come out in the past few months.
t is hard to overstate the significance of the new results on Alzheimer's disease
that have come out in the past few months.
For decades scientists have known that there are large amounts of a protein called beta-amyloid in the brains of patients with Alzheimer's disease. We can measure it chemically in our instruments. We can observe it with special radioactive dyes that bind to it in the brains of living patients. But we have no idea what it's there for.
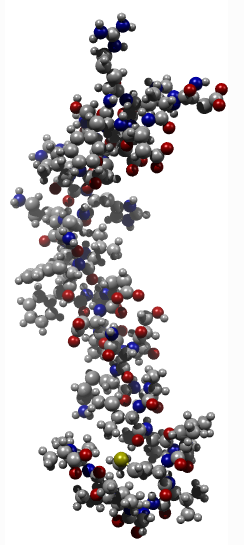
3D model of β-amyloid
β-amyloid is what scientists call a sticky protein. There are many sticky proteins, and biochemists hate them because they're hard to work with. In general, sticky proteins are used to create structures in the cell. Actin, for instance, forms long girder-like structures that make up the cytoskeleton, and its stickiness helps other proteins attach to it.
Many years ago, I found that one of the proteins β-amyloid binds to is a signaling protein called 14-3-3. My theory was that Alzheimer's disease happened when the brain attempted to repair injury, and that somehow the repair went haywire. I planned to continue this study. By finding what β-amyloid binds to, I hoped, we could identify its function.
Unfortunately, the non-profit place I worked for was only interested in finding new drugs that could bring in cash. My boss forced me to change the conclusions in my paper to pretend I had found a therapeutic. I ended up abandoning my research.
Now researchers at Harvard and elsewhere have finally found what may be the real function of β-amyloid: to defend against invading microorganisms. It's a fantastic result and a beautiful theory. It seems that the pieces are falling into place.
Microglia
The first piece is the discovery that microglia are responsible for the synapse loss in Alzheimer mouse models[1]. Microglia are the immune cells of the brain. They secrete a great many molecules, such as BDNF, which induces repair of neurons. They also produce proteins called C1q and C3, which are members of the classical complement cascade, a complicated process involving some 25 different proteins that self-assemble on cell surfaces, causing cell lysis and bringing death to invading microorganisms.
During brain development, many more synapses are created than are needed. The brain uses the same mechanism to get rid of them: C1q and C3 proteins localize to synapses and eliminate them by a process called phagocytosis[2]. During development, cells called astrocytes release signals that induce the expression of C1q and C3 in the brain. These proteins attach to synapses, tagging them for elimination, and the microglia engulf them, destroying them as if they were invading pathogens.[3]
So, for some unknown reason, it appears that, in Alzheimer's disease, the brain's own protective mechanism sees its own synapses as alien invaders.
Interestingly, microglia are also known to function differently in men and women, at least as far as pain is concerned. This might explain the greater incidence of Alzheimer's in women.
Synapse loss
Stevens and colleagues at Harvard are finding evidence that this same process of eliminating excess synapses may have somehow become aberrantly reactivated in neurodegenerative disease. We've known for a long time that synapse loss is one of the earliest signs of Alzheimer's disease. By eliminating healthy synapses, the brain is erasing its own memories.
As often happens, other labs are discovering the same thing. A lab at the Hong Kong University of Science and Technology (HKUST) has reported that interleukin-33 tends to counteract the pathogenesis of Alzheimer's disease[4]. This suggests that something may be going wrong with many aspects of signaling in the neuroimmune system. Many other researchers, too numerous to name here, have found critical pieces of this puzzle.
A similar process could even be occurring in schizophrenia[5], another disease where synapse loss figures prominently.
Infection
But what would trigger such a thing? And how does β-amyloid fit in? The second piece of that puzzle has just been found. Deepak Kumar and colleagues in Moir's and Tanzi's labs at Harvard have discovered that β-amyloid protects against microbial infection. [6]
β-amyloid has long been known to form clumps known as oligomers that kill neurons. But its real function may be to function as an antibiotic. Kumar et al. found that salmonella bacteria infection in the brains of mice caused a rapid increase in β-amyloid deposition that surround the microorganism and kill it.
There are lots of questions that still need to be answered. Is Alzheimer's disease really triggered by a brain infection, or is it a signaling error? What triggers the microglia synapse elimination program?
We don't know yet. And of course it doesn't mean a cure is on the way. But these results explain some big mysteries: in a small percentage of patients, a genetic mutation causes large amounts of β-amyloid to be produced. But after all these years, we still aren't sure why the other 98–99% of patients have so much β-amyloid. That is still a mystery. But now, at last, we might know what it does.
References
1. Hong S, Beja-Glasser V, Nfonoyim B, Frouin A, Li S, Ramakrishnan S, Merry K, Shi Q, Rosenthal A, Barres B, Lemere C, Selkoe D, Stevens B (2016). Complement and microglia mediate early synapse loss in Alzheimer mouse models. Science 352(6286):712–716 Link
2. B. Stevens, N. J. Allen, L. E. Vazquez, G. R. Howell, K. S. Christopherson, N. Nouri, K. D. Micheva, A. K. Mehalow, A. D. Huberman, B. Stafford, A. Sher, A. M. Litke, J. D. Lambris, S. J. Smith, S. W. John, B. A. Barres (2007). The classical complement cascade mediates CNS synapse elimination. Cell 131, 1164–1178. Link
3. Stephan AH, Barres BA, Stevens B. (2012). The complement system: an unexpected role in synaptic pruning during development and disease. Annu Rev Neurosci. 2012;35:369–89. Link
4. Fu AK, Hung KW, Yuen MY, Zhou X, Mak DS, Chan IC, Cheung TH, Zhang B, Fu WY, Liew FY, Ip NY. (2016) IL-33 ameliorates Alzheimer's disease-like pathology and cognitive decline. Proc Natl Acad Sci U S A. 113(19):E2705–13. Link
5. Sekar A, Bialas AR, de Rivera H, Davis A, Hammond TR, Kamitaki N, Tooley K, Presumey J, Baum M, Van Doren V, Genovese G, Rose SA, Handsaker RE; Schizophrenia Working Group of the Psychiatric Genomics Consortium, Daly MJ, Carroll MC, Stevens B, McCarroll SA. plus 307 other collaborators (2016). Schizophrenia risk from complex variation of complement component 4. Nature. 2016 Feb 11;530(7589):177–183. Full version (paywall) Link
6. Kumar DK, Choi SH, Washicosky KJ, Eimer WA, Tucker S, Ghofrani J, Lefkowitz A, McColl G, Goldstein LE, Tanzi RE, Moir RD. (2016). Amyloid-beta peptide protects against microbial infection in mouse and worm models of Alzheimer's disease. Sci Transl Med. 2016 May 25;8(340):340ra72. Link