 harmacologists often say that their industry is the ultimate test of a biological
theory. But what happens when a drug that's supposed to do one thing actually
does another?
harmacologists often say that their industry is the ultimate test of a biological
theory. But what happens when a drug that's supposed to do one thing actually
does another?
There's increasing evidence that if there's a beneficial effect of statins, it's not due to lowering of cholesterol but due to its anti-inflammatory activity.[1,2,3] What this means is unclear. Is atherosclerosis an autoinflammatory disorder? Or is inflammation, like high cholesterol, a symptom of something else, perhaps some as-yet undiscovered pathogen?
The adaptive immune system (T- and B-cells) get screwed up. Examples: type 1 diabetes, rheumatoid arthritis, multiple sclerosis
Autoinflammatory disordersThe innate immune system (monocytes, macrophages, and neutrophils) is screwed up. Examples: familial Mediterranean fever, type 2 diabetes
Let's look back to see why people thought cholesterol was the culprit in cardiovascular disease. A typical study was from Sever et al. in 2008.[4] At first glance it seems to support the cholesterol hypothesis. The study, which was funded by Pfizer (the maker of atorvastatin), claimed to show that atorvastatin was effective. Below is their Figure 2A. Does it show a change in cholesterol?
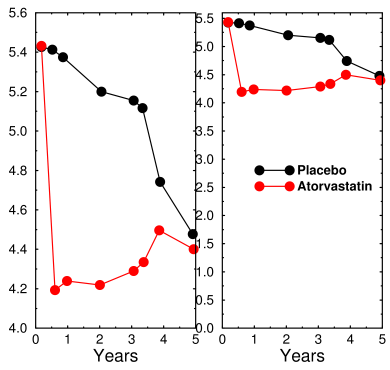
Atorvastatin effect on cholesterol.Left: as presented by Sever et al., Right: correctly drawn graph with y-axis starting at 0 shows that cholesterol was actually reduced by 24 percent.
The left panel shows how the graph appeared in the paper. Notice that the Y axis starts at 4.0, making it appear that there's a big change. In fact, when plotted correctly (at right) it's clear that the drug only reduced plasma cholesterol by 24%. It also reduced LDL (not shown) by 35%.
Because of the huge number of patients (4500 placebos and 5100 treated) the result is hugely statistically significant. But is it clinically significant? Well, it turns out that this change is only about three times the daily variation.[5] Whether that's clinically significant depends on whether cholesterol has a causal relationship to cardiovascular disease.
(The sharp drop in cholesterol in the placebos happened because the study was terminated after three years and the placebo patients were allowed to take statins.)
Skeptics sometimes argue about the statistics: the heart attack rate in the placebo group was 3.1% while the rate in the statin group was 2%. The authors claimed a 36% reduction in risk, while the skeptics call it 1.1%.
These statistical quandaries are important, but they miss the bigger picture. Statins are a classic example of what happens when you assume your drug is doing only what you want. I've seen this over and over, even in the trials I was involved in. There's an old joke in pharmacology: a drug is only specific when it's new.
In one trial, I tried to convince my boss that his drug was not as specific as he thought. Drugs don't bind to proteins; they bind to specific regions on proteins, called motifs or binding domains. Many different proteins, sometimes with opposite functions, contain the same binding domain. For example, the EF Hand domain always binds calcium. There are 62 different proteins that contain a C1 domain, which binds a certain lipid molecule. The guy wouldn't hear of it. To this day, he still can't understand why the results weren't what he hoped for.
The same thing happened in schizophrenia research. Antipsychotics appeared to back up the dopamine hypothesis. It wasn't until their effects on the innate immune system were observed that the dopamine theory finally was abandoned.
Does this matter? As long as it benefits the patient, why care? The problem is that a partial success turns a result into a dogma. Statins were thought of as wonder drugs and were spectacularly profitable. Patients were told in no uncertain terms that they needed them in order to live. Statin results emboldened doctors to say that eating eggs and meat was killing millions of people. Even as evidence accumulated that lowering plasma cholesterol was merely a side-effect, proponents of alternative explanations found that their theories aroused little interest. Hundreds of researchers accepted the cholesterol theory, which is now known to be false, and abandoned other lines of research.
Scientists expect to have papers rejected if they make a mistake. But when reviewers reject their papers because reviewers think the problem has been solved and the new idea is simply beating a dead horse, scientists have little choice but to abandon the new idea.
Heart disease is far from cured: US cardiovascular mortality rates for women have increased steadily since 1979 and passed men in 1983. The trend for men has been downward since about 1968, well before the approval of lovastatin in 1987, due to a decline in smoking and improvements in acute care. If researchers had spent those years figuring out what statins were really doing, we might be a lot closer today to knowing the true cause of cardiovascular disease. Maybe we'd even have a cure.
We need more effort at unbiased drug screening, either by better computer modeling or by improved screening assays, to identify alternative mechanisms of action. Otherwise the statin problem will continue to happen, and we'll get more dead-ends.
1. Liberale L, Carbone F, Montecucco F, Sahebkar A. (2020). Statins reduce vascular inflammation in atherogenesis: A review of underlying molecular mechanisms. Int J Biochem Cell Biol. 122, 105735. doi: 10.1016/j.biocel.2020.105735.
2. Antonopoulos AS, Margaritis M, Lee R, Channon K, Antoniades C. (2012). Statins as anti-inflammatory agents in atherogenesis: molecular mechanisms and lessons from the recent clinical trials. Curr Pharm Des. 18(11), 1519–1530. Link PMID: 22364136 PMCID: PMC3394171 DOI: 10.2174/138161212799504803
3. Kwak BR, Mulhaupt F, Mach F. (2003). Atherosclerosis: anti-inflammatory and immunomodulatory activities of statins. Autoimmun Rev. 2(6), 332–338. Link PMID: 14550874 DOI: 10.1016/s1568-9972(03)00049-1
4. Sever PS, Poulter NR, Dahlof B, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes G, Mehlsen J, Nieminen MS, O'Brien ET, Ostergren J; ASCOT Investigators (2008). The Anglo-Scandinavian Cardiac Outcomes Trial lipid lowering arm: extended observations 2 years after trial closure. Eur Heart J. 29(4):499–508. doi: 10.1093/eurheartj/ehm583.
5. Hegsted DM, Nicolosi RJ (1987). Individual variation in serum cholesterol levels. Proc Natl Acad Sci U S A. 84(17), 6259–6261. doi: 10.1073/pnas.84.17.6259 PMCID: PMC299050 PMID: 3306674
mar 15 2020, 5:11 am. edited mar 16 2020, 6:50 am
