 used an online symptom checker last week and it diagnosed me as a hypochondriac.
I had all the symptoms—literally. Bada bump.
used an online symptom checker last week and it diagnosed me as a hypochondriac.
I had all the symptoms—literally. Bada bump.
We need a word for the opposite of hypochondriac—a person who thinks they're perfectly healthy when they're really not—because that's what doctors are creating. Talking to your doctor these days is like talking to a criminal prosecutor. A prosecutor's job is to nail people for committing a crime. There are so many laws the only rational response is to keep schtum. Now doctors are getting in on the act.
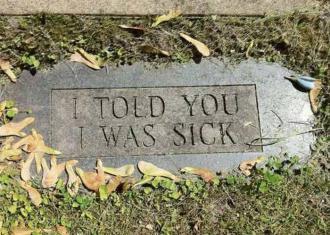
Tombstone of the unknown hypochondriac (source unknown)
Doctors have a new rule saying they must ask if you're getting enough food, if you're a victim of violence, if you feel like you want to do away with yourself or commit violence, and on and on. Say yes to any of them, and two burly guys might come in and drag you down to the O.R. while you're saying “I'm not dead! I'm getting better. I feel happy!”
Then there's the testing: nowadays doctors won't stop testing you until they find something wrong. Thanks to the lawyers, they get sued if they miss something, but not if they find something that's not there. Over-aggressive treatment is the result.
Hospitals keep close tabs on the most dangerous procedures, like general anesthesia, but there's a growing realization that the risk of iatrogenic illness may be greater then previously realized. Here's a case report about something that happened to a friend of mine last year.
A witty and kindly middle-aged secretary was seriously overweight and had surgery to replace a painful knee joint. When she returned, it was clear something had gone horribly wrong. She could not speak above a whisper. Then she was out for a couple weeks with pneumonia. She seemed to recover, but a few weeks later she was dead.
People shouldn't die of aspiration pneumonitis after knee surgery. It can only be explained as a complication of anesthesia. General anesthesia has been compared to getting hit by a truck, and that is a good description of how it affects people. Global anesthesia puts the patient in a medically induced coma. It's traumatic for the brain. It could be argued that any death within a few weeks of surgery can be attributed to anesthesia, but the disease, not the treatment, always gets blamed.
Aspiration pneumonitis is a risk if the patient eats food less than 6 to 8h before surgery. The acidic stomach contents are regurgitated and enter the trachea and lung. Vomiting cannot occur during the coma stage, but may occur in the induction stages or during recovery. Vomiting occurs in up to 30% of all post-operative patients. The belief is that the risk is low because the patient is awake. But something better is needed.
One alternative is spinal anesthesia, or neuraxial blockade, where the anesthetic is injected into the subdural or epidural space. It has a low risk but it's catastrophic when something occurs[1]. Over 19% of patients 60–69 yrs have lumbar canal stenosis, which increases the risk of permanent spinal injury. Infection can also occur, leading to meningitis, often confused with post-LP headache, showing up a few weeks after the surgery.
These complications are rare—2 to 4 per 100,000—but transient symptoms, especially from spinal lidocaine, happen between 4 and 36% of the time. The longer the procedure, the greater risk from anesthesia, and that includes conventional anesthesia. This can include heart attack, postoperative confusion, and stroke. Whether it triggers dementia is in dispute.
Few realize that the treatment for prostate cancer, androgen deprivation therapy, increases the risk of Alzheimer's disease by 2.3x[2]. Likewise, in women, hormone replacement therapy that starts more than five years after menopause increases the risk, while therapy started immediately reduces the risk. It's almost as if the body senses when its reproductive life is over and self-destructs.
I should mention that cause and effect are not yet firmly established for the prostate cancer risk, and some studies dispute the findings.
Hospitals worry that mentioning the risks will produce public hysteria, but it's been estimated that 20–30% of patients receive contraindicated care. In a 2000 JAMA commentary, Dr Barbara Starfield of the Johns Hopkins School of Hygiene and Public Health claimed[3] that between 225,000 and 284,000 Americans die each year from iatrogenic causes, the biggest factors being medical errors, nosocomial infections (infections picked up in hospitals), and ‘non-error’ adverse effects of medications. Some reports[4] claimed even higher numbers, but they were based on some pretty slippery data.
The ongoing push by the US government to nationalize the health insurance industry, with the ultimate goal of nationalizing healthcare itself, makes all figures suspect. In the JAMA commentary, Starfield was actually pushing for universal health insurance. Thus the issue is political, so we cannot know to what extent the numbers are exaggerated.
Nonetheless, the numbers were picked up by naturopaths and alternative medicine fanatics. In many medical articles we often find overly rosy assessments and skewed statistics. These conflicting claims create anti-vaxxers and naturopaths who over-react and assume the worst.
Where I work, they sent out a notice saying if we don't get an influenza vaccine we're automatically fired. Nobody ever thought that several thousand terrified staff would suddenly smash down the doors trying to get vaccinated. I had a drugstore immunize me; my employer lost the records and nagged me for twenty minutes pressuring me to get another shot.
The biggest risk of all this is that the more prying questions you ask, the more the patient feels like he's in a roach motel and keeps schtum. While your doctor is operating on you to cure some mosquito bite or pumping you full of SSRIs because you foolishly told them you were depressed, something sinister and nasty is going to remain undiagnosed.
I just know I have pneumonoultramicroscopicsilicovolcaniosis. Also subacute sclerosing panencephalitis and meningoencephalomyeloradiculopathy. But I'm not telling them. My hypochondria is a thing of the past. I am cured!
1. Hewson DW, Bedforth NM, Hardman JG. (2018). Spinal cord injury arising in anaesthesia practice. Anaesthesia. Jan;73 Suppl 1:43–50. doi: 10.1111/anae.14139. PMID: 29313911
2. Nead KT, Gaskin G, Chester C, Swisher-McClure S, Leeper NJ, Shah NH. (2017). Association Between Androgen Deprivation Therapy and Risk of Dementia. JAMA Oncol. Jan 1;3(1):49–55. doi: 10.1001/jamaoncol.2016.3662. PMID: 27737437
3. Starfield B (2000). Is US Health Really the Best in the World? JAMA. 2000;284(4):483–485. doi:10.1001/jama.284.4.483 (paywalled, but can be found by search)
4. Makary MA, Daniel M (2016). Medical error—the third leading cause of death in the US. BMJ 2016;353:i2139
feb 15 2020, 5:43 am
