 had a good laugh last week when the UK Daily Mail, living down to its reputation
as the most unreliable news site on the Internet, started claiming that President
Trump now has “roid rage“ after getting a shot of dexamethasone for his
Covid-19.
had a good laugh last week when the UK Daily Mail, living down to its reputation
as the most unreliable news site on the Internet, started claiming that President
Trump now has “roid rage“ after getting a shot of dexamethasone for his
Covid-19.
That claim is hardly worth refuting, but for the record dexamethasone is a glucocorticoid, not an anabolic androgenic steroid. It does not cause roid rage, although there is one report in the scientific literature about how it interferes with female mating preference, making them more sexually aggressive. But that's only true, as far as anyone knows, in lizards (though maybe it's worth investigating in humans, for purely scientific reasons). So maybe that's what the newspaper is claiming: the Orange One is actually a lizard person.
Glucocorticoids
Glucocorticoids may not be the most exciting molecules at the moment, and they're not the safest thing to use against a virus, but they're widely prescribed for their ability to suppress the immune system. For example, prednisolone is sometimes used to treat alopecia, an autoimmune disorder that causes hair loss in young people. Their side effects include facial hair growth in females, irritability, and ‘moon face,’ in which the entire face becomes round.
There are some celebrities out there who have shown evidence that they've been treated with that one, which makes sense because there are many different autoimmune disorders, including multiple sclerosis, lupus, rheumatoid arthritis, psoriasis, and atopic dermatitis. But how do they work?
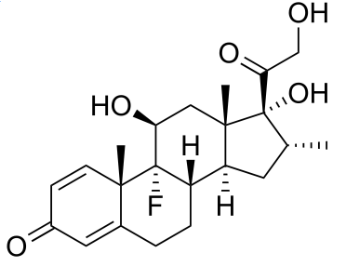
Dexamethasone
Corticosteroids are, of course, made from cholesterol. Specialized proteins such as STARD1, STARD3. and TSPO (aka translocator protein) move the cholesterol to the inner mitochondrial membrane, where cholesterol is converted to pregnenolone. It then gets converted to progesterone, then to corticosterone, and ultimately to cortisol, which is the main glucocorticoid in humans. In periods of stress, a part of the hypothalamus in the brain called the paraventricular nucleus releases CRH (corticotropin releasing hormone), which goes to the pituitary which releases POMC (proopiomelanocortin) and ACTH. The ACTH then goes to the adrenal glands to stimulate cortisol secretion. Glucocorticoids inhibit the production of these molecules.
Yes yes, I hear you saying, everybody knows that, it is basic endocrinology 101, but how does that suppress inflammation? It seems they work through cellular receptors. When cortisol binds to a receptor, it stops the cell from producing inflammatory cytokines, which are magical pixie-like proteins that do very complex, mischievous, and sometimes contradictory things to the immune system. There are also several kinds of cortisol receptors, and they all affect cytokines in different ways. It also turns out that CRH isn't just made in the hypothalamus as originally thought; CRH is also made in the skin, eyes, adipose tissue, ovaries, uterus, thymus, bladder, liver, stomach, and kidney.
Resolvins
But the big excitement out there is about resolvins, which are a completely different way of stopping inflammation. Resolvins are made in the body from DHA (docosahexaenoic acid) and eicosapentaenoic acid, which are fatty acids sold in health food stores as nutritional supplements. Human physiology being ridiculously complex, there are many different resolvins, protectins, maresins, and lipoxins, collectively called specialized pro-resolving mediators or SPMs. According to what we know so far they all act through receptors, and micro-RNAs or miRNAs, of which there are so many they are given numbers instead of names, are somehow involved [1]. Glucocorticoids like dexamethasone, which was given to Trump, work in a somewhat similar way. [2,3]
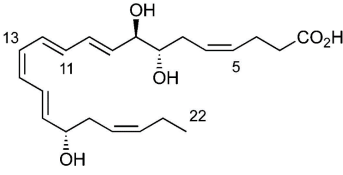
Resolvin D1
People have vast amounts of DHA in their brain already, where it's conjugated into phospholipids in their cell membranes. DHA constitutes 50% of your neuronal cell membrane. So taking more DHA would have little or no effect unless you have a deficiency (which could happen if you, say, avoid eating fatty food, but surely no one would ever do that).
What makes resolvins interesting is the connection to aspirin. Aspirin is unlike every other anti-inflammatory drug. It covalently modifies COX-2, which is the enzyme that manufactures PGE2 (prostaglandin E2), an inflammatory pain molecule. But it doesn't just block COX-2—it transforms it in some bizarre way so that instead of making pro-inflammatory molecules, it makes resolvins, which are anti-inflammatory, although slightly different from normal resolvin.
Resolvins are especially found in polymorphonuclear leukocytes or polymorphonuclear neutrophils, which are cells in your bloodstream that kill invading cells by engulfing them and then blasting them with poisons known as reactive oxygen species, after which they can change into macrophages that clean up the resulting mess. They seemed to be more effective with long-term inflammation, such as that occurring in cancer, atherosclerosis, and even possibly Parkinson's and Alzheimer's disease, than with the acute inflammation in Covid-19. Until now.
Obesity and COVID-19
COVID-19 can trigger many types of autoimmune and autoinflammatory diseases, including lupus erythematosus, alopecia, Kawasaki disease, and Guillain-Barré, antiphospholipid, and and pediatric inflammatory multisystemic syndromes. [4,5] But the reasons why this happens are obscure.
Last month a bombshell paper[5] came out saying that obesity, which is probably the biggest risk factor for COVID-19, causes a loss of SPMs. Obesity doubles the risk of having COVID-19, which is surprising since you might think obese people would have an ample supply of DHA in their adipocytes. It's not entirely clear what is going on, and the authors do an awful lot of speculating—in fact, the entire paper is mostly speculation—but a SPM called protectin DX was able to increase survival of mice with H5N1 (a terrible, lethal form of influenza) while antivirals had no effect. SPMs have a major advantage over steroids in that they aren't immunosuppressive, which means they don't increase the risk of opportunistic infections or other side effects. Which means, if it's true, that the doctors at Bethesda could have just given Trump an aspirin and told him to call them in the morning.
I suspect Trump probably would have tweeted about it, in which case the press would report that he's advocating intravenous aspirin as a treatment and we would all have to stop taking it because everyone suddenly remembered it is a deadly poison.
Update (Oct 27 2020)
A paper just came out in Anesthesia and Analgesia [7] describing a retrospective observational study saying that patients on aspirin had a lower risk of needing ventilation. They say there was no difference in bleeding or thrombosis, but they still attribute the aspirin effect to anticoagulation rather than its anti-inflammatory effect. The actual changes, while statistically significant, were small (35.7% aspirin vs 48.4% non-aspirin, p=0.03), but after adjusting for confounding variables the changes became highly significant (ventilation HR 0.56, p=0.007, ICU admission HR 0.57, p=0.005, and in-hospital mortality HR 0.53, p=0.02).
As expected, this study elicited a flood of comments about how deadly low-dose aspirin is. People just don't want this disease to go away.
1. Recchiuti A (2013). Resolvin D1 and its GPCRs in resolution circuits of inflammation. Prostaglandins Other Lipid Mediat. Dec;107:64–76. doi: 10.1016/j.prostaglandins.2013.02.004. Epub 2013 Mar 15. PMID: 23500003 (paywalled)
2. Mohammadi L, Mosayyebi B, Imani M, Zarghami N, Alizadeh E, Rahmati M (2020). Correlation between Dexamethasone and miRNAs in the regulation of apoptosis, drug-resistance, and metastasis of cancer cell. Curr Mol Med. Sep 25. doi: 10.2174/1566524020666200925155614. PMID: 32981504 DOI: 10.2174/1566524020666200925155614
3. Kim D, Nguyen QT, Lee J, Lee SH, Janocha A, Kim S, Le HT, Dvorina N, Weiss K, Cameron MJ, Asosingh K, Erzurum SC, Baldwin WM 3rd, Lee JS, Min B (2020). Anti-inflammatory Roles of Glucocorticoids Are Mediated by Foxp3+ Regulatory T Cells via a miR-342-Dependent Mechanism. Immunity Sep 15;53(3):581–596.e5. doi: 10.1016/j.immuni.2020.07.002. PMID: 32707034
4. Galeotti C, Bayry J (2020). Autoimmune and inflammatory diseases following COVID-19. Nat Rev Rheumatol. Aug;16(8):413–414. doi: 10.1038/s41584-020-0448-7. PMID: 32499548; PMCID: PMC7271827.
5. Rodríguez Y, Novelli L, Rojas M, De Santis M, Acosta-Ampudia Y, Monsalve DM, Ramírez-Santana C, Costanzo A, Ridgway WM, Ansari AA, Gershwin ME, Selmi C, Anaya JM. Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. J Autoimmun. 2020 Jun 16:102506. doi: 10.1016/j.jaut.2020.102506. PMID: 32563547; PMCID: PMC7296326.
6. Pal A, Gowdy KM, Oestreich KJ, Beck M, Shaikh SR (2020). Front Immunol. Aug 11, 11:1997. Obesity-Driven Deficiencies of Specialized Pro-resolving Mediators May Drive Adverse Outcomes During SARS-CoV-2 Infection. PMID: 32983141 PMCID: PMC7438933 DOI: 10.3389/fimmu.2020.01997 Link
7. Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, McCurdy MT, Tabatabai A, Kumar G, Park P, Benjenk I, Menaker J, Ahmed N, Glidewell E, Presutto E, Cain S, Haridasa N, Field W, Fowler JG, Trinh D, Johnson KN, Kaur A, Lee A, Sebastian K, Ulrich A, Peña S, Carpenter R, Sudhakar S, Uppal P, Fedeles BT, Sachs A, Dahbour L, Teeter W, Tanaka K, Galvagno SM, Herr DL, Scalea TM, Mazzeffi MA (2020). Aspirin Use is Associated with Decreased Mechanical Ventilation, ICU Admission, and In-Hospital Mortality in Hospitalized Patients with COVID-19. Anesth Analg. Oct 21. doi: 10.1213/ANE.0000000000005292. PMID: 33093359. Link
oct 10 2020, 8:46 am Updated October 27, 2020 6:26 am
