he connection between cannabis use and psychosis, which means hallucinations,
delusions, and disordered thoughts, is well established. It follows a dose-response
curve, which is solid evidence that cannabis is responsible and that frequent
users have a higher risk [1]. So reefer madness is real, although
most people who use cannabis don't have psychotic reactions. But which comes
first: the reefer or the madness? And who is at risk?
he connection between cannabis use and psychosis, which means hallucinations,
delusions, and disordered thoughts, is well established. It follows a dose-response
curve, which is solid evidence that cannabis is responsible and that frequent
users have a higher risk [1]. So reefer madness is real, although
most people who use cannabis don't have psychotic reactions. But which comes
first: the reefer or the madness? And who is at risk?
One recent epidemiologic study [3] found that the rates of self-reported psychosis increase by 2.5-fold and correlate with the use of cannabis, while non-users did not report increased psychosis over the same period.
One could argue, of course, that cannabis use somehow makes people more likely to falsely report themselves as being psychotic. Or maybe they were somehow unable to maneuver their computer mouse to click the right answer. These experiments are not easy to do.
Whoa-a-a-a, I can feel my DNA, dude
Another way of assessing causality is by searching for genetic differences known as polymorphisms. This is called a genome-wide association study or GWAS. And indeed, genetic polymorphisms (which differ from ordinary mutations in that they're present in many people) were found in COMT (an enzyme that degrades dopamine), DRD2 (dopamine receptor D2), and DAT (dopamine active transporter). However, another GWAS study found no such changes, and the authors suggested [3] that the studies implicating dopamine could have been influenced by the pre-existing dopamine theory of schizophrenia.
Another study [4] found that while genetic polymorphisms that put a person at risk for schizophrenia robustly correlated with cannabis usage, the statistics did not suggest a causal effect but rather that the same genetic factors that induced cannabis use also contributed to schizophrenia.
Writing in the American Journal of Psychiatry [5], Suhas Ganesh and Deepak Cyril D'Souza concluded that while much of the evidence supports the theory that cannabis causes psychosis and that the risk of conversion to schizophrenia is greater than with other psychomimetic drugs, other evidence suggests a reverse-causal mechanism, whereby schizophrenia-related mechanisms lead to cannabis use. The debate is still ongoing.
Play it faster
It seems unimaginable, given the unpleasant nature of its effects—not to mention the risk of psychosis and loss of long-term memory—that nearly 200 million people worldwide and over 15% of the US population voluntarily use cannabis each year. Its effects range from disorientation, confusion, disordered perceptions, to acute paranoid psychosis. But how does it work?
Cannabis contains a variety of bioactive compounds, many of which act on the brain. The three main ones are:
THC (Δ9-tetrahydrocannabinol) Hindley et al.[6] say “A single THC administration induces psychotic, negative, and other psychiatric symptoms with large effect sizes.” We can only speculate about why that happens: most sources only say it interferes with the flow of signals between neurons, which is not really an explanation. Many other drugs can induce psychosis, though cannabinoids are said to be more effective than other drugs at inducing schizophrenia.
THC induces both “positive” symptoms such as hallucinations and psychosis-like delusions, thought disorder, and “negative” symptoms like blunted emotions, anhedonia, amotivation, depression, and cognitive impairment. The terms 'positive' and 'negative' don't refer to the desirability of the symptoms but whether the effect was added or taken away.
CBD (cannabidiol) CBD is an anti-inflammatory agent. It has been suggested that modern cannabis is more able to induce psychosis because the ratio of THC to CBD is increasing [7] due to the prevalence of the sinsemilla or unseeded female form, which contains 14% THC but almost no CBD [8], suggesting that CBD protects against THC.
However, CBD does not induce mental symptoms and some authors say it does not affect the effects of THC [6]. If that is true, then the question remains: has something else besides potency changed to make marijuana more dangerous?
Cannabigerol is also an anti-inflammatory agent but is less potent than CBD. It was found to reduce neuronal loss by half in patients with Huntington's disease.[9]
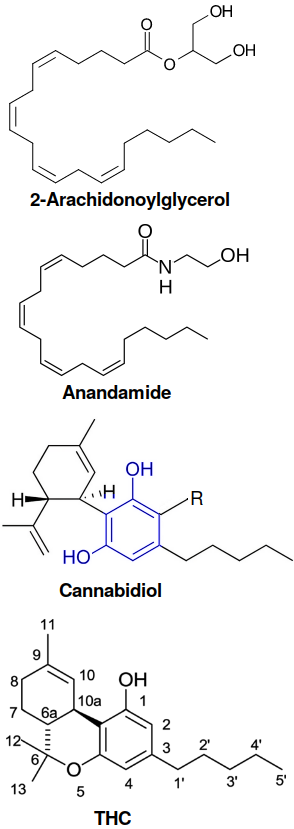
Structure of endocannabinoids, Δ9-THC, and CBD. Endocannabinoids have the double bond structure of arachidonic acid, an N-6 polyunsaturated fatty acid. Phytocannabinoids like CBD (where R=H) and THC have a resorcinol ring structure shown in blue. Nearly 200 cannabinoids are known. The double bond in THC is essential for binding to CB1 and CB2 receptors; only Δ9-THC, Δ8-THC, and the aromatized form (cannabinol or CBN) are psychoactive. Just to make things fun, the carbons of CBD and THC are numbered differently because its fused heterocycle structure takes precedence over the isoprenoid moiety[15]
Endocannabinoid's not here, man
One reason THC and CBD work is that they bind to the same receptors as endogenous cannabinoids. Unlike phytocannabinoids (CBD and THC), which are meroterpenoids, or “partial” terpenoids containing a resorcinyl (1,3-dihydrobenzene) core structure and a dihydropyran ring, endocannabinoids are straight-chain unsaturated lipid molecules made in the brain from arachidonic acid. The two most important endocannabinoids are:
Anandamide (arachidonoyl ethanolamide)
2-arachidonoylglycerol
It's like, the immune system, man
The endocannabinoid system has many functions. One of the most important is modulation of the immune system.[10,11]
A big clue with THC is that strong mental effects only occur by the second dose, suggesting that either receptor activation or an immune response is involved. Many researchers think the immune system may also be involved in schizophrenia. Indeed, Dalmau and Graus wrote an interesting book detailing how the symptoms of an autoimmune disorder called anti-NMDA receptor encephalitis are indistinguishable from those of schizophrenia. They reanalyzed samples from several patients who had been diagnosed with schizophrenia and found that in fact they did not have schizophrenia, but anti-NMDA receptor encephalitis.
CBD suppresses the innate immune system by inhibiting a number of pathways [10] and thus acts as an anti-inflammatory agent. CBD also triggers myeloid-derived suppressor cells, which suppress T cell activity.
Δ9THC too may have anti-inflammatory effects. Endocannabinoids and phytocannabinoids bind to a variety of receptors, including endocannabinoid receptors CB1 and CB2, the peroxisome proliferator-activated receptor PPARγ, and several others.
Anti-inflammatory effects are not always desirable. Cannabis suppresses JAK/STAT signaling in T cells, thereby suppressing antitumor activity,[12] potentially increasing the risk for cancer. Cannabis use has also been associated with hypersensitivity to allergens such as molds, dust mites, cat dander, and many types of plants including rye grass, oak, and peanut. [13]
Researchers in Chiba, Japan found that activation of the CB receptors increased Iba1 (ionized calcium-binding adapter molecule 1) in the brain after mice were given LPS, a highly inflammatory molecule secreted by gut microbiota.[14] The job of Iba1 is to reorganize actin, which makes up the structure of the cell, to facilitate phagocytosis by microglia. So it seems that THC can also increase the activity of the innate immune system.
One might speculate that if an immune response is somehow involved in producing cannabis intoxication, then persons in young adulthood, when schizophrenia is most likely to strike, could be pushed over the edge if they possess the genetic risk factors. This remains to be demonstrated, and the universality of those risk factors needs to be established before anyone can offer genetic screening to cannabis users.
[1] Robinson T, Ali MU, Easterbrook B, Hall W, Jutras-Aswad D, Fischer B. Risk-thresholds for the association between frequency of cannabis use and the development of psychosis: a systematic review and meta-analysis. Psychol Med. 2022 Mar 24:1–11. doi: 10.1017/S0033291722000502. PMID: 35321777.
[2] Livne O, Shmulewitz D, Sarvet AL, Wall MM, Hasin DS. Association of Cannabis Use-Related Predictor Variables and Self-Reported Psychotic Disorders: U.S. Adults, 2001–2002 and 2012–2013. Am J Psychiatry. 2022 Jan;179(1):36–45. doi: 10.1176/appi.ajp.2021.21010073. PMID: 34645275; PMCID: PMC8945254.
[3] Carvalho C, Vieira-Coelho MA. Cannabis induced psychosis: A systematic review on the role of genetic polymorphisms. Pharmacol Res. 2022 Jul;181:106258. doi: 10.1016/j.phrs.2022.106258. PMID: 35588917.
[4] Johnson EC, Hatoum AS, Deak JD, Polimanti R, Murray RM, Edenberg HJ, Gelernter J, Di Forti M, Agrawal A. The relationship between cannabis and s chizophrenia: a genetically informed perspective. Addiction. 2021 Nov;116(11):3227–3234. doi: 10.1111/add.15534. PMID: 33950550; PMCID: PMC8492483.
[5] Ganesh S, D'Souza DC. Cannabis and Psychosis: Recent Epidemiological Findings Continuing the "Causality Debate". Am J Psychiatry. 2022 Jan;179(1):8–10. doi: 10.1176/appi.ajp.2021.21111126. PMID: 34974754. https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2021.21111126
[6] Hindley G, Beck K, Borgan F, Ginestet CE, McCutcheon R, Kleinloog D, Ganesh S, Radhakrishnan R, D'Souza DC, Howes OD. Psychiatric symptoms caused by cannabis constituents: a systematic review and meta-analysis. Lancet Psychiatry. 2020 Apr;7(4):344–353. doi: 10.1016/S2215-0366(20)30074-2. PMID: 32197092; PMCID: PMC7738353.
[7] Potter DJ, Clark P, Brown MB. Potency of delta 9-THC and other cannabinoids in cannabis in England in 2005: implications for psychoactivity and pharmacology. J Forensic Sci. 2008 Jan;53(1):90–94. doi: 10.1111/j.1556-4029.2007.00603.x. PMID: 18279244.
[8] Potter DJ, Hammond K, Tuffnell S, Walker C, Di Forti M. Potency of Δ9 -tetrahydrocannabinol and other cannabinoids in cannabis in England in 2016: Implications for public health and pharmacology. Drug Test Anal. 2018 Apr;10(4):628–635. doi: 10.1002/dta.2368. PMID: 29441730. anandamide
[9] Valdeolivas S, Navarrete C, Cantarero I, Bellido ML, Muñoz E, Sagredo O. Neuroprotective properties of cannabigerol in Huntington's disease: studies in R6/2 mice and 3-nitropropionate-lesioned mice. Neurotherapeutics. 2015 Jan;12(1):185–199. doi: 10.1007/s13311-014-0304-z. PMID: 25252936; PMCID: PMC4322067.
[10] Anil SM, Peeri H, Koltai H. Medical Cannabis Activity Against Inflammation: Active Compounds and Modes of Action. Front Pharmacol. 2022 May 9;13:908198. doi: 10.3389/fphar.2022.908198. PMID: 35614947; PMCID: PMC9124761.
[11] Anil SM, Peeri H, Koltai H. Medical Cannabis Activity Against Inflammation: Active Compounds and Modes of Action. Front Pharmacol. 2022 May 9;13:908198. doi: 10.3389/fphar.2022.908198. PMID: 35614947; PMCID: PMC9124761.
[12] Xiong X, Chen S, Shen J, You H, Yang H, Yan C, Fang Z, Zhang J, Cai X, Dong X, Kang T, Li W, Zhou P. Cannabis suppresses antitumor immunity by inhibiting JAK/STAT signaling in T cells through CNR2. Signal Transduct Target Ther. 2022 Apr 6;7(1):99. doi: 10.1038/s41392-022-00918-y. PMID: 35383142; PMCID: PMC8983672.
[13] Min JY, Min KB. Marijuana use is associated with hypersensitivity to multiple allergens in US adults. Drug Alcohol Depend. 2018 Jan 1;182:74–77. doi: 10.1016/j.drugalcdep.2017.09.039. PMID: 29172121.
[14] Wan X, Eguchi A, Qu Y, Yang Y, Chang L, Shan J, Mori C, Hashimoto K. Gut-microbiota-brain axis in the vulnerability to psychosis in adulthood after repeated cannabis exposure during adolescence. Eur Arch Psychiatry Clin Neurosci. 2022 Jun 6. doi: 10.1007/s00406-022-01437-1. PMID: 35666299.
[15] Hanuš LO, Meyer SM, Muñoz E, Taglialatela-Scafati O, Appendino G. Phytocannabinoids: a unified critical inventory. Nat Prod Rep. 2016 Nov 23;33(12):1357-1392. doi: 10.1039/c6np00074f. PMID: 27722705.
jul 11 2022, 6:25 am