 his week the biggest health threat of the year is finally past. I
refer, of course, to the end of deer season, which ended last Saturday,
spreading peace, silence, and absence of bullet holes in brown-colored
objects across the country. Deer have come out of hiding, mostly asymptomatic,
which is to say apparently healthy and free of bullet holes.
his week the biggest health threat of the year is finally past. I
refer, of course, to the end of deer season, which ended last Saturday,
spreading peace, silence, and absence of bullet holes in brown-colored
objects across the country. Deer have come out of hiding, mostly asymptomatic,
which is to say apparently healthy and free of bullet holes.
But are they really? Recent thinking seems to be that you can diagnose a disease by PCR without ever seeing the patient. If we could devise a suitable PCR test we might find those deer are all dying of undetectable bullet wounds.
There are grave risks in discussing this: if you express skepticism about COVID-19, you will be accused of murder if someone around you dies. And for sure you will be censored by Google and social media. On Twitter you might even get a Trigger Warning saying you're talking about something controversial.
By definition an asymptomatic patient does not cough, have a fever, feel sick, or have a positive CT scan. In one study 57% of ‘asymptomatic’ patients had no symptoms at all. [6] So it might seem that an asymptomatic patient is an oxymoron.
The WHO defines an asymptomatic case as a laboratory-confirmed case without overt symptoms. One review paper claims that “Asymptomatic individuals carrying SARS-CoV-2 are hidden drivers of the pandemic” and claims that up to 81% of COVID-19 infections are asymptomatic.[1] But as with PCR Ct results, asymptomatic transmission is probabilistic.
Transmissibility of COVID is a hot topic (10,197 articles so far in the medical literature) and a bonanza for testing labs: Luxembourg and the state of Bavaria in Germany are testing their entire population. Our university has started randomly testing 10% of their staff and student population each week. But does a ‘positive’ PCR test constitute a case?
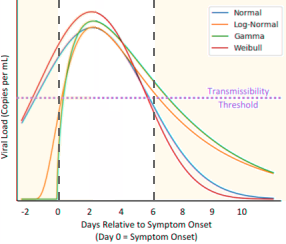
Theoretical graph of viral load as a function of time (modified from Savvid et al. fig. 2 [2]) The authors say the transmissibility threshold is 106 copies per mL [4], which corresponds to a Ct of 24.[5] Transmission is only possible when the viral load is above the dotted line. Depending on the mathematical model, there may or may not be such a thing as presymptomatic transmission.
The question is difficult to answer because asymptomatic and presymptomatic overlap. The medical profession is outsourcing its duty to diagnose to clinical labs, creating a distinction between a ‘case’ for reporting and a ‘case’ deserving of treatment. This is leading to widespread confusion: one study in China failed to find any transmission from asymptomatic patients, while others find it a major source of infection. A meta-analysis [2] of 34 studies made the following observations:
- There is significant publication bias.
- Nasopharyngeal swabs are unreliable. (This suggests that blood samples rather than swabs would be a better indication of infection.)
- Some studies failed to distinguish presymptomatic from asymptomatic.
- Publicly available lists of symptoms continually change, so people may believe themselves symptomatic when they are not. Older individuals experience various aches and pains all the time and may fail to identify symptoms when they appear.
- The relationship between PCR testing and infectivity is not yet clear, with many studies finding that virus can be extracted only from patients with Ct below 24.
Conclusions
There seems to be agreement that asymptomatic COVID-19 may indeed exist, but the quality of much of the research has been dismal. In particular, Internet fact-checkers have contributed to hysteria and produced a skeptical reaction against the hysteria that is becoming more extreme.
There is also considerable uncertainty regarding the likelihood of transmission. Here is the conclusion of a meta-analysis in The Lancet [3] of the effectiveness of face masks:
Face mask use could result in a large reduction in risk of infection (n=2647; aOR [adjusted odds ratio] 0.15, 95% CI 0.07 to 0.34, RD −14.3%, −15.9 to −10.7; low certainty), with stronger associations with N95 or similar respirators compared with disposable surgical masks or similar (eg, reusable 12–16-layer cotton masks; pinteraction = 0.090; posterior probability >95%, low certainty). Eye protection also was associated with less infection (n=3713; aOR 0.22, 95% CI 0.12 to 0.39, RD −10.6%, 95% CI −12.5 to −7.7; low certainty).
This is a fancy way of saying they don't know the answer. The authors say “randomized trials are needed to better inform the evidence.” But saying you don't know the answer won't get you into The Lancet.
You might argue, considering the rubbish that gets published there, that this is a good thing, but it's true for all journals. This is called publication bias and it prevents an entire class of possible conclusions. As with negative results, unknowability is itself an valuable finding.
1. Nikolai LA, Meyer CG, Kremsner PG, Velavan TP. Asymptomatic SARS Coronavirus 2 infection: Invisible yet invincible. Int J Infect Dis. 2020 Nov;100:112-116. doi: 10.1016/j.ijid.2020.08.076. PMID: 32891737; PMCID: PMC7470698.
2. Savvides C, Siegel R. Asymptomatic and presymptomatic transmission of SARS-CoV-2: A systematic review. medRxiv [Preprint]. 2020 Jun 17:2020.06.11.20129072. doi: 10.1101/2020.06.11.20129072. PMID: 32587980; PMCID: PMC7310638.
3. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020 Jun 27;395(10242):1973-1987. doi: 10.1016/S0140-6736(20)31142-9. PMID: 32497510; PMCID: PMC7263814. Full text link
4. Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M, Bleicker T, Brünink S, Schneider J, Ehmann R, Zwirglmaier K, Drosten C, Wendtner C. Virological assessment of hospitalized patients with COVID-2019. Nature 2020 May;581(7809):465–469. doi: 10.1038/s41586-020-2196-x. PMID: 32235945.
5. He D, Zhao S, Lin Q, Zhuang Z, Cao P, Wang MH, Yang L. The relative transmissibility of asymptomatic COVID-19 infections among close contacts. Int J Infect Dis. 2020 May;94:145-147. doi: 10.1016/j.ijid.2020.04.034. PMID: 32315808; PMCID: PMC7166025.
6. Rivett L, Sridhar S, Sparkes D, Routledge M, Jones NK, Forrest S, Young J, Pereira-Dias J, Hamilton WL, Ferris M, Torok ME, Meredith L; CITIID-NIHR COVID-19 BioResource Collaboration, Gupta R, Lyons PA, Toshner M, Warne B, Bartholdson Scott J, Cormie C, Gill H, Kean I, Maes M, Reynolds N, Wantoch M, Caddy S, Caller L, Feltwell T, Hall G, Hosmillo M, Houldcroft C, Jahun A, Khokhar F, Yakovleva A, Butcher H, Caputo D, Clapham-Riley D, Dolling H, Furlong A, Graves B, Gresley EL, Kingston N, Papadia S, Stark H, Stirrups KE, Webster J, Calder J, Harris J, Hewitt S, Kennet J, Meadows A, Rastall R, Brien CO, Price J, Publico C, Rowlands J, Ruffolo V, Tordesillas H, Brookes K, Canna L, Cruz I, Dempsey K, Elmer A, Escoffery N, Jones H, Ribeiro C, Saunders C, Wright A, Nyagumbo R, Roberts A, Bucke A, Hargreaves S, Johnson D, Narcorda A, Read D, Sparke C, Warboys L, Lagadu K, Mactavous L, Gould T, Raine T, Mather C, Ramenatte N, Vallier AL, Kasanicki M, Eames PJ, McNicholas C, Thake L, Bartholomew N, Brown N, Parmar S, Zhang H, Bowring A, Martell G, Quinnell N, Wright J, Murphy H, Dunmore BJ, Legchenko E, Gräf S, Huang C, Hodgson J, Hunter K, Martin J, Mescia F, O'Donnell C, Pointon L, Shih J, Sutcliffe R, Tilly T, Tong Z, Treacy C, Wood J, Bergamaschi L, Betancourt A, Bowyer G, De Sa A, Epping M, Hinch A, Huhn O, Jarvis I, Lewis D, Marsden J, McCallum S, Nice F, Curran MD, Fuller S, Chaudhry A, Shaw A, Samworth RJ, Bradley JR, Dougan G, Smith KG, Lehner PJ, Matheson NJ, Wright G, Goodfellow IG, Baker S, Weekes MP. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020 May 11;9:e58728. doi: 10.7554/eLife.58728. PMID: 32392129; PMCID: PMC7314537.
dec 11 2020, 6:31 am
