 t's been over thirty years since the association between beta-amyloid and
Alzheimer's disease was discovered[1]. Hundreds of millions of dollars have been
spent trying to get it out of the brain. We now have several ways of doing it,
but the effect on the disease has been minimal. Yet somehow, this theory Just.
Won't. Die.
t's been over thirty years since the association between beta-amyloid and
Alzheimer's disease was discovered[1]. Hundreds of millions of dollars have been
spent trying to get it out of the brain. We now have several ways of doing it,
but the effect on the disease has been minimal. Yet somehow, this theory Just.
Won't. Die.
Here's the background. There are a lot of facts here, but stay with me.
There are two types of Alzheimer's disease (which I'll call AD for short): early-onset and late-onset, also called familial and sporadic. The early-onset type is inherited, and it's always caused by a mutation in one of three proteins: APP (amyloid precursor protein), presenilin 1, or presenilin 2. Early onset means they get sick as early as their 30s. The vast majority of patients are late onset, where only people over 65 get it.
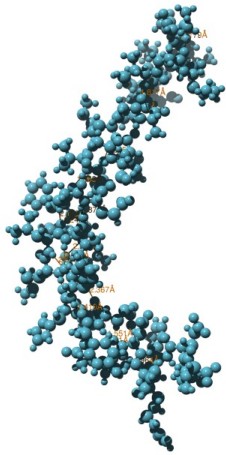
Beta-amyloid (Aβ), maybe not as evil as we thought. (Monomer)
AD patients have massive amounts of beta-amyloid, or Aβ, in their brains. I've measured this myself. With PET scanning, doctors can even visualize it in patients. Mice have been created that have these mutations, and like AD patients, they too get massive amounts of Aβ and they die with symptoms sort of resembling AD. But unlike humans, it seems that almost everything we do to these mice cures them.
That tells us that we need better models for AD, and everyone recognizes it. Even so, it would be a mere cloud on the horizon except for the fact that Aβ is now a diagnostic criterion for AD. The definition has become almost circular: if there are no Aβ plaques, pathologists often won't call it AD. We know there are many elderly patients, and patients with brain injuries, who have Aβ but not AD. There could even be patients out there with AD but no Aβ. If there are, we may never know about them.
Update (May 5, 2018): BACE1 inhibitors don't work
Beta-amyloid is made from big membrane protein called APP. Part of APP, called the extracellular domain, sticks out from the cell membrane, and it's this part that gets chopped up by two extracellular proteases called secretases. First BACE1 or β-secretase cuts it, then γ-secretase. γ-Secretase is a big complex containing several proteins, the most important one being presenilin-1.
In 2013, Eli Lilly and a host of prestigious universities reported[17] that semagacestat, a presenilin-1 inhibitor, didn't work against AD. In 2017, Merck abandoned verubecestat, a BACE-1 inhibitor. The report finally appeared on May 3, 2018[18].
It was known going in that both of these drugs would be toxic, but for most people those toxic effects, even cancer, would be a small price to pay considering the alternative. Who wouldn't in a heartbeat trade the possibility of death by cancer for the certainty of death by dementia? Semagacestat caused weight loss, cancer, infections, and a host of laboratory abnormalities in the patients. These are called adverse events or AEs, which were so severe the researchers terminated the phase 3 trial early. Verubecestat was also toxic, and caused suicidal ideation, falls and injuries, and weight loss; this trial was terminated for futility after 50 months of trying.
The final blow comes from the antibody clinical trials. One antibody, aducanumab, dramatically reduced the amount of Aβ in the brain, but there was no statistically significant effect on the dementia score[3]. Bigger trials are planned, and everyone hopes that maybe, unlike the previous trials, this one will work.
These clinical trials represent billions of dollars and millions of man-hours spent testing the beta-amyloid theory. The toxicity of the inhibitors could be explained by the fact that β-secretase and γ-secretase also do other things besides making beta-amyloid, but the theory could not have gotten a more definitive test: if beta-amyloid was causing the disease, these inhibitors and antibodies would have reversed it or at least slowed its progression.
So let's consider what we have: a molecule that takes two steps to synthesize. It accumulates in AD, and if we put tiny concentrations of it on our cultured neurons it kills them. If we put it in mice, their memory is impaired. Yet if we remove it from our patients, either by blocking one of the steps needed to make it, or if we remove it with an antibody, the disease continues to get worse until the patient dies, as if nothing had changed.
Presenilin
Another substantive blow to the Aβ theory comes from in vitro studies on presenilin. There are 228 known mutations of presenilin 1 that have been found in AD. Most of them prevent the enzyme γ-secretase, of which presenilins are a part, from working. For years, it was dogma that presenilin mutations increase the amount of Aβ or the ratio of the two forms of Aβ (42 and 40). But last year a group in Beijing[2], in a monumental effort, cloned 138 of these mutations and found it was not true. Nothing correlated: not the age of onset, not the amount of enzyme activity remaining, not even the ratio. Most of the mutations actually decreased Aβ.
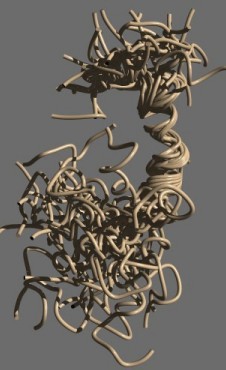
Beta-amyloid 1–42 (Aβ42). Ensemble structure of 30 molecules modeled by Tomaselli et al. from NMR data[13]. Rendered in Chimera
Here's another problem: until recently, you couldn't get a grant on AD unless you could relate it to Aβ. If you wrote a paper on AD, you had to pay obeisance to Aβ. That's starting to change, but industry is still focused on Aβ, and some companies still won't pay attention to you unless you have something that lowers Aβ.
Metal ions
There are, of course, a few mavericks out there who have other theories. One idea was that Aβ does something to metal ions, like copper, zinc, iron, or aluminum. This makes sense since Aβ has a divalent metal binding site.
These theories are somewhat disreputable, and I feel dirty even mentioning aluminum. That's a shame, because many people don't realize how complex and interesting aluminum chemistry is. Aluminum metal is not absorbed very well in the intestine or by inhalation. It reacts rapidly with oxygen to aluminum oxide, which is biologically inert. There are also ionized forms, mainly Al3+, which turns into insoluble aluminum hydroxide at normal pH. In the lab, other forms of aluminum are used that are highly reactive.
Aluminum encephalopathy can occur in dialysis patients, and it causes oxidative stress (a chemical phenomenon not related to the kind of stress a person can feel), which is also seen in AD. But the symptoms of aluminum encephalopathy are totally different from those of AD[4], and epidemiological studies have ruled it out.[5]
Similar fates have befallen the copper and zinc theories: copper chelation therapy failed miserably in clinical trials.
Apolipoprotein E and cholesterol
If not Aβ or an environmental toxin, then what? I have this table taped over my desk, and I've been staring at it every day for months.
| ApoE | Percent of | Percent in patients | Age of | ||
|---|---|---|---|---|---|
| Genotype | population | Male | Female | Combined | Onset |
| E2/E2 | 0.7 | 0 | 0 | 0 | >85 |
| E2/E3 | 10.1 | 28 | 11 | 16 | >85 |
| E2/E4 | 2.3 | 50 | 0 | 20 | >85 |
| E3/E3 | 65.1 | 7 | 29 | 20 | 83 |
| E3/E4 | 17.9 | 37 | 54 | 48 | 76 |
| E4/E4 | 3.3 | 91 | 91 | 91 | 68 |
If viewing on a cell phone, drag table left or right to scroll.
Apolipoprotein E, or ApoE for short, is a protein that carries cholesterol around in the brain and elsewhere. The numbers in the table are very typical. For example, we once found that 8 of our 10 patients who had been healthy were E3/E3 and the other two were E2/E3. By contrast, only 4 out of 10 of our AD group were E3/E3. Five were E3/E4 and one was E4/E4.
The largest genetic factor in late onset AD is ApoE4. We all have two copies, or alleles, of ApoE, and there are three main forms (2,3, and 4), so there are six possible genotypes you could have. About 13% of people have at least one ApoE4 allele[6]. The table shows that if you have one copy, it increases your risk by 3.7×; if you have two, it increases your risk by 12-fold[7]. In this study, 91% of the people with two copies eventually got the disease. Half got it by age 68. It's a catastrophe happening before our eyes.
But there's a problem here, too. First, it's yet another “bad protein” theory which we're so fond of. You could live without ApoE, though your cholesterol levels would be sky-high, and even with two good copies, many people still get the disease. And second, what can you do about ApoE? Cutting dietary cholesterol wouldn't help: the brain makes its own. ApoE doesn't bind Aβ as once thought—we now know that the only interaction is by competing with LRP-1, which is one of ApoE's receptors. One group is trying to develop drugs that convert E4 into E3. I'm glad it's not me. It would be a fiendishly difficult task.
There are also, as you might guess, lots of studies trying to connect ApoE with Aβ: maybe ApoE4, the bad form, causes it to aggregate, or maybe it interferes with its clearance. These experiments are difficult; even the basic question of whether Aβ clearance is impaired in AD is disputed. Everybody cites one paper that used mass spectrometry that purported to show it[8], but I'm not convinced it's right.
Getting a solid understanding of why Aβ is increased in AD is essential. The body has many ways of making sure every protein stays at the correct level. Why should this one be different? Oligomerized Aβ—that is, tiny soluble clumps of it—is hundreds of times above its normal concentration.[14] We're still not sure why.
The assumption is that the oligomers, once formed, can't be removed. If so, we still need to know why they are formed in the first place, and why the microglia don't clear them away. The assumption is that they form spontaneously because there's so much Aβ, which somehow blocks the clearance mechanism. A “vicious circle” is often suggested, but a vicious circle is not a good explanation: why does the vicious circle start, and what stops it from dying out? Oligomers, monomers, and maybe plaques are in equilibrium.[15,16] Monomers are fairly innocuous, as are mature plaques, so the theory is circular. A lot more research is needed here.
Inflammation, Tau, and Rare coding variants
There are other theories as well: inflammation is a prominent feature of AD. Maybe, one theory goes, it's not just a by-product of neurodegeneration, but a cause. Another theory says that brain injury or some other factor is causing the neurons to try to divide, but since they're neurons this is forbidden, and so the neurons die. And, lurking in the background, are the so-called Tauists, waiting for their theory about Tau protein to hit the big time.
Last month a paper came out in Nature Genetics describing some new “rare coding variants” in AD. What is a rare coding variant? Is this really a “cure” as the news media are portraying it?
The article was titled “Rare coding variants in PLCG2, ABI3 and TREM2 implicate microglial-mediated innate immunity in AD.”[9] That title seemed eerily familiar to me, and sure enough I had two very similar papers on my computer already:
- Rare coding variants in phospholipase D3 PLD3 confer risk for Alzheimers disease[10]
- Rare variants in PLD3 do not affect risk for early onset Alzheimer disease in a European Consortium Cohort[11]
This sort of thing happens a lot: two groups studying the same thing come to opposite conclusions. Too often we just assume the more recent study is the correct one, but in fact all it shows is that more research is needed.
A rare coding variant is nothing more than a mutation that occurs in a small number of people. These studies are important because they show that people have finally started looking for something else besides Aβ. The tool they're using is called a genome-wide association study or GWAS[12]. The idea is that if some mutation increases the risk, it would give us a clue as to what's going on.
Interestingly enough, some of the authors of these three papers are the same. That may just be a coincidence: the PLCG2 paper has 117 authors. The list of authors and affiliations is 4 pages of fine print. Why? Maybe it's a huge amount of work. Or maybe it just takes a battalion and truckloads of ammo to kill a theory that led an entire field astray for three frickin' decades.
References
1. Glenner GG, Wong CW. (1984). Alzheimer's disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 120, 885–890. Link
2. Sun L, Zhou R, Yang G, Shi Y (2017). Analysis of 138 pathogenic mutations in presenilin-1 on the in vitro production of Abeta42 and Abeta40 peptides by gamma-secretase. Proc Natl Acad Sci U S A. 114, E476–E485 Link
3. Sevigny J, Chiao P, Bussière T, Weinreb PH, Williams L, Maier M, Dunstan R, Salloway S, Chen T, Ling Y, O'Gorman J, Qian F, Arastu M, Li M, Chollate S, Brennan MS, Quintero-Monzon O, Scannevin RH, Arnold HM, Engber T, Rhodes K, Ferrero J, Hang Y, Mikulskis A, Grimm J, Hock C, Nitsch RM, Sandrock A (2016). The antibody aducanumab reduces Aβ plaques in Alzheimer's disease. Nature 537, 50—56. Link Correction
4. Lidsky TI (2014). Is the aluminum hypothesis dead? J Occup Environ Med 56(5 Suppl), S73–S79.
5. Rondeau V (2002). A review of epidemiologic studies on aluminum and silica in relation to Alzheimer's disease and associated disorders. Rev Environ Health 17, 107–121.
6. Ordovas JM, Litwack-Klein L, Wilson P, Schaefer M, Schaefer E (1987) Apolipoprotein E isoform phenotyping methodology and population frequency with identification of apoEl and apoE5 isoforms. J Lipid Res 28, 371–380.
7. Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA. (1983). Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science 26, 921–923. 8. Mawuenyega KG, Sigurdson W, Ovod V, Munsell L, Kasten T, Morris JC, Yarasheski KE, Bateman RJ (2010). Decreased clearance of CNS beta-amyloid in Alzheimer's disease. Science 330, 1774. Link
9. Sims R et al. (2017). Rare coding variants in PLCG2, ABI3, and TREM2 implicate microglial-mediated innate immunity in Alzheimer's disease. Nat Genet. 2017 Jul 17. doi: 10.1038/ng.3916. Link
10. Cruchaga C, Karch CM, Jin SC, Benitez BA, Cai Y, Guerreiro R, Harari O, Norton J, Budde J, Bertelsen S, Jeng AT, Cooper B, Skorupa T, Carrell D, Levitch D, Hsu S, Choi J, Ryten M, Sassi C, Bras J, Gibbs RJ, Hernandez DG, Lupton MK, Powell J, Forabosco P, Ridge PG, Corcoran CD, Tschanz JT, Norton MC, Munger RG, Schmutz C, Leary M, Demirci FY, Bamne MN, Wang X, Lopez OL, Ganguli M, Medway C, Turton J, Lord J, Braae A, Barber I, Brown K; Alzheimer's Research UK (ARUK) Consortium, Pastor P, Lorenzo-Betancor O, Brkanac Z, Scott E, Topol E, Morgan K, Rogaeva E, Singleton A, Hardy J, Kamboh MI, George-Hyslop PS, Cairns N, Morris JC, Kauwe JSK, Goate AM (2014). Rare coding variants in the phospholipase D3 gene confer risk for Alzheimer's disease. Nature 505, 550–554. Link
11. Cacace R, Van den Bossche T, Engelborghs S, Geerts N, Laureys A, Dillen L, Graff C, Thonberg H, Chiang HH, Pastor P, Ortega-Cubero S, Pastor MA, Diehl-Schmid J, Alexopoulos P, Benussi L, Ghidoni R, Binetti G, Nacmias B, Sorbi S, Sanchez-Valle R, Lladó A, Gelpi E, Almeida MR, Santana I, Tsolaki M, Koutroumani M, Clarimon J, Lleó A, Fortea J, de Mendonça A, Martins M, Borroni B, Padovani A, Matej R, Rohan Z, Vandenbulcke M, Vandenberghe R, De Deyn PP, Cras P, van der Zee J, Sleegers K, Van Broeckhoven C; Belgium Neurology (BELNEU) Consortium and the European Early-Onset Dementia (EU EOD) Consortium (2015). Rare Variants in PLD3 Do Not Affect Risk for Early-Onset Alzheimer Disease in a European Consortium Cohort. Hum Mutat. 2015 Dec;36(12):1226-35. doi: 10.1002/humu.22908. Epub 2015 Oct 14. Link
12. Cuyvers E, Sleegers K. Genetic variations underlying Alzheimer's disease: evidence from genome-wide association studies and beyond. Lancet Neurol. 15, 857–868. Link
13. Tomaselli S, Esposito V, Vangone P, van Nuland NA, Bonvin AM, Guerrini R, Tancredi T, Temussi PA, Picone D. (2006). The alpha-to-beta conformational transition of Alzheimer's Abeta-(1-42) peptide in aqueous media is reversible: a step by step conformational analysis suggests the location of beta conformation seeding. Chembiochem. 7, 257–267.
14. Yang T, Li S, Xu H, Walsh DM, Selkoe DJ (2016). Large Soluble Oligomers of Amyloid beta-Protein from Alzheimer Brain Are Far Less Neuroactive Than the Smaller Oligomers to Which They Dissociate. J Neurosci 37, 152–163.
15. Nag S, Sarkar B, Bandyopadhyay A, Sahoo B, Sreenivasan VK, Kombrabail M, Muralidharan C, Maiti S. (2011). Nature of the amyloid-beta monomer and the monomer-oligomer equilibrium. J Biol Chem. 286, 13827–13833.
16. Bitan G, Lomakin A, Teplow DB (2001). Amyloid beta-protein oligomerization: prenucleation interactions revealed by photo-induced cross-linking of unmodified proteins. J Biol Chem. 276, 35176–35184.
17. Doody RS, Raman R, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, He F, Sun X, Thomas RG, Aisen PS; Alzheimer's Disease Cooperative Study Steering Committee, Siemers E, Sethuraman G, Mohs R; Semagacestat Study Group (2013). A phase 3 trial of semagacestat for treatment of Alzheimer's disease. N Engl J Med. 25;369(4):341–350. doi: 10.1056/NEJMoa1210951.
18. Egan MF, Kost J, Tariot PN, Aisen PS, Cummings JL, Vellas B, Sur C, Mukai Y, Voss T, Furtek C, Mahoney E, Harper Mozley L, Vandenberghe R, Mo Y, Michelson D (2018). Randomized Trial of Verubecestat for Mild-to-Moderate Alzheimer's Disease. N Engl J Med. 378(18):1691–1703. doi: 10.1056/NEJMoa1706441.
aug 12, 2017; updated May 05, 2018, 4:28 am; edited may 12 2018
